Malaria
Malaria an acute, chronic, systemic, mosquito-borne tropical disease characterized by chills and fever, anaemia, and often serious or fatal complications. Malaria exhibits a wide range of clinical manifestations which arise from the destruction of red blood cells and the resultant disruption of metabolism. The disease, characterized by ferbrile attacks, secondary anaemia, and splenic enlargement, tends to progress from an acute to chronic state. During the acute stage, there are intermittent ferbrile episodes, and during the subsequent chronic stage, periods of latency broken by series of relapses resembling the acute primary attack. The severity and persistence depend upon many factors, including the species and strain of the parasite, the resistance of the patient, and the environment.
Distribution and prevalence 'Malaria is a worldwide disease, and there are probably more cases of it than of any other infection. Though the popular mind usually associates malaria with tropical or subtropical climates, such is not the case; Sweden, Finland, and northern Russia have, in the past, been subject to serious epidemics. Whether or not malaria existed in North America prior to the discovery of the continent has not been definitely established; however, this disease was evidently recognised as a factor in colonization on the Massachusetts coast and the Gorgia-Carolina coast as early as middle of the seventeenth century. Even in 1930s, there were six to seven million cases annually in the continental United States. Hypoendemic areas are found in South China, Southeast Asia, Indonesia, India and Asia Minor. Malaria does not occur in certain islands such as, islands of the Central and South Pacific, the Galapagos islands, Guam, the Hawaiian and Midway Islands, and also in New Zealand.
The disease is most prevalent in low humid regions and coastal areas, and is less frequent in deserts and mountainous regions. Its occasional presence has been reported at altitude of about 3,000 metres in South America, Asia, and East Africa. Its distribution is determined by the presence of its mosquito vector.
For the past 75 years, however, the disease has been declining in many parts of the world. Europe, once widely malarious, is now in large part free from the disease, and South America can entertain hopes of its eradication. In the United States, fewer than 10 proven cases of natural malarial transmission by mosquitoes were reported in 1957. In India it was estimated at mid 20th century that malaria was still killing 1 million persons annually. It was estimated by PF Russel (1943, Bull. New York Acad. Med. 19: 599-630) that not less than 3 million malarial deaths, and at least 30 million cases of malarial fever occur per year throughout the world.
Malaria at one time considered as one of the most important and disabilitating disease of mankind, became rare during 1970s even in many previously malarious countries of the world. The eradication programmes successfully brought the disease under control. Dramatically, rooted out in the 1960s, the malarial parasite has returned with a vengeance. The World Health Organisation recently (2000) estimates that more than 100 countries, and 40 percent of the world's population are now at risk. Every year, this mosquito-borne infection strikes 300-500 million people of whom 1.5-2.7 million die. Experts and researchers find a link between climate changes and the resurgence of malaria that was once written off.
History 'Although the name 'malaria' was not employed until the middle of the eighteenth century, the disease is one of the most ancient of infections known to man. Hippocrates as early as 5th century BC divided periodic fevers into quotidian (daily), tertian (alternate days), and quartan (fever three days apart) types. He observed that those who drank the stagnant marsh water had large stiff spleens, a characteristic of the disease, and fetal dropsy was common among them. The fable of Hercules and Hydra is believed to refer to malaria. In 1753 Torti named the disease 'malaria', believing it to be air-borne and emanating from the bad air (mal aria) rising from swamps and marshes. Credit for the discovery of causal agent (1880) belongs to Laveran, a French army surgeon who was then stationed in Algeria. Although the mosquito transmission theory is said to have been held for many years by Italian and Tyrolese peasants, and the natives of what was formerly German East Africa, the first well-formulated mosquito-malaria theory was advanced by King in 1883. In 1885 and 1886, Golgi discovered that the course of the fevers corresponded to the development of the parasite in the blood corpuscles and particularly to their periodic sporulation. He demonstated this for both the quartan and tertian parasites.
Sir Patrick Manson, British pioneer in tropical medicine, stated in 1894 that he suspected the mosquito to be the vector (carrier) of malaria. It was his sustained guidance and encouragement that carried Sir Donald Ross, the British physian on to those brilliant discoveries in India in 1897-98 that definitely incriminated mosquitoes as vectors of malaria, and twice won for him the Nobel Prize. Although Ross made important discoveries in the field of human malaria and its anopheline vector, his chief discovery was the complete life cycle of the causal organism of bird malaria in a culicine mosquito; he established the bird-to-mosquito-to-bird cycle. In November 1898 the Italian investigators A Bignani, GB Grassi, and G Bastianelli first infected man by mosquitoes, described the full development in man and noted that malaria is probably transmitted only by anophiline mosquito, an observation that continues to hold true. Subsequently, numerous scientists and researchers proved beyond doubt that several species of Anopheles are the vectors, and three species of Plasmodium are the causal organisms of malaria.
For therapy, a major event was the mass cultivation of strains of cinchona trees giving high yields of quinine alkaloids. This was achieved by the Duch in the East Indies. In 1891 Guttman and Paul Ehrlich found therapeutic effects of methylene blue against malaria. During World War I, Schulemann and his associates discovered plasmochin which culminated in the production of quamaquine in 1924. Several other anti-malarial drugs including mepacrine were discovered during World War II. With passage of time improved synthetic compounds appeared for treatment of malaria replacing the old ones.
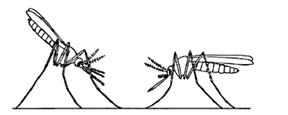
Malarial parasite' The malarial parasite is a protozoon of genus Plasmodium. Four species produce malaria in humans: P. vivax, P. ovale, P. malariae, and P. falciparum. To survive and to multiply, the malarial parasite needs two hosts-the man and the female anopheles mosquito. The mosquito is known as 'vector' because through it the disease is transmitted from one person to other. The parasite is introduced into the human body through the bite of an infected female anopheles. Within half an hour of the bite, the parasite passes to the liver through blood circulation and there it multiplies. This cycle of the life of the parasite is known as 'exoerythrocytic cycle'. After a few days, the parasite leaves the liver and invades the red blood cells or erythrocytes. Here another round of multiplication, called 'erythrocytic cycle' takes place. Soon the RBC, overloaded with parasites, explodes releasing a mass of parasites. Toxic substances are also released. The patient shivers and becomes feverish.
In many cases the patient with malaria may experience a few days of continuous fever before developing the classical bouts or fever with shivering. In case of vivax and ovale malaria, fever occurs on alternate days. P. malariae causes fever every third day. But with P. falciparum, the fever has no particular pattern. The infected RBC stick to the lining of small blood vessels leading to the brain, kidney, liver, lungs, and gut. The patient with impaired consciousness and convulsion may enter into a state of comma. This is what is known as the 'cerebral malaria'. The patient may die within few hours.
Usually the malarial patients feel chilled when temperature is rising. The mercury may rise as high as 104 F. After 30 minutes to an hour, the so-called hot or flush phase begins. It lasts for several hours, at the end of which the patient begins to sweat profusely. Simultaneously, the fever goes down. The cycle is repeated over and over again. Apart from fever, the patient becomes anaemic and the liver and spleen show symptoms of enlargement.
The vector mosquitoes' Thirty four anopheline mosquitoes have been recorded in Bangladesh, of which seven species are found transmitting malaria in this country. Out of these 7 vectors, four species, Anopheles dirus, A. philippinensis, A. sundaicus and A. minimus are considered important malaria vectors. The rest three species, A. aconitus, A. annularis and A. vagus have been incriminated recently (1991-1993) in places where malaria outbreaks took place.
A. dirus is found transmitting malaria in hilly forested and foot hill areas in eastern part of Bangladesh. This wild species is largely an out-door resting mosquito and bites mainly in the middle part of night. It is difficult to find adults in dwellings during daytime. The members of this species seem to rest a while before feeding and leaves soon after feeding for out-door shelters. They equally bite man out-door.
A. minimus, characteristically a species of the forested hills and foot-hill areas and considered as the primary malaria vector, was virtually eliminated after DDT spraying during Malaria Eradication Programme (MEP) in 1960s. It starts feeding just after sunset, but attacks more after midnight. It is generally regarded as a domestic mosquito. Recently, there is sign of reappearance of this species in low density, probably due to the long absence of any insecticidal pressure.
A. philippinensis is a malaria vector of flood-plain deltaic region of Bangladesh. It is now scarcely found specially after DDT spraying during MEP. The other possible reason of gradual disappearance of this species may be attributed to the gradual shrinkage of its favourable breeding places such as marshy land, ground pools, ditches, tanks, ponds etc. This species is now mainly seen resting in cattle sheds or on vegetation around outdoor shelters, rarely found indoors.
A. sundaicus is found transmitting malaria in coastal areas of Bangladesh. It virtually disappeared after DDT spraying. Presently, it is found in low numbers in coastal areas including Cox's Bazar. It breeds in brackish-water.
A. annularis, A. vagus and A. aconitus are found present in some particular flood-plain areas of Bangladesh. These 3 species are generally regarded as a cattle feeder, occasionally biting man. A. annularis is usually found in large numbers and may have certain importance as a malaria vector in some localities. A. aconitus is not common and may be regarded as a secondary vector of malaria in some particular areas of Bangladesh. A. vagus, a fairly common species of mosquito at all places of Bangladesh, has recently been incriminated as a malaria vector. Strangely, it is not a malaria vector in India. These species may have started playing a role in malarial transmission in the changed ecological situation and are found to transmit vivax malaria in areas where previously A. philippinensis acted as a vector. High density of these 3 species in some particular season or in some particular ecological situation may play a role in disease transmission, specially in outbreak.
Malaria incidence' In Bangladesh, malaria has always been a major public health problem. It is still endemic in the northern and eastern parts bordering India and Myanmar. Outbreaks of malaria are also being reported from those areas as well as from some pockets of flood plain deltoid areas of Bangladesh. The malaria situation has been deteriorating since 1988. Incidence of reported cases rose from 33,824 cases in 1988 to 60,023 in 1998, and 70% of them being Plasmodium falciparum infection; 53,808 (90%) of the cases were recorded in greater Chittagong and Chittagong Hill Tracts Districts, and out of which 42,222 were caused by falciparum malaria (70.34% of all falciparum infection in the country). The districts most affected by falciparum malaria are Rangamati, Khagrachari, Bandarban, Cox's Bazar, and Chittagong.
It is observed that malaria morbidity and mortality are high among the people who are transferred from non-endemic zone, and are settled in the greater district of Chittagong and Chittagong Hill Tracts. Even in Dhaka City cases are often reported. In fact most cases of this disease go unreported and many patients fail to contact with an organised health service of any sort.
Malaria vector control situation' Prior to 1920, there were no anti-malaria activities in Bangladesh. In 1920, the Department of Public Health started functioning, but very little activities were carried out during 1920 to 1947, except some anti-larval measures in a piece-meal manner, limited to a few urban and rural areas. With the establishment of the Malaria Eradication Programme (MEP) in 1960s, anti-mosquito measures were carried out by spraying indoors with DDT where the vector species usually rest before and after taking blood meal. The programme progressed well till 1970 and the number of reported malaria cases came down to 6,660 in 1970. The MEP suffered during liberation war in 1971, and after that it never came up as before.
The present strategy mostly deals with the detection of malaria cases and to give a prompt clinical treatment. Measures against vectors are almost non-existent, and DDT spraying has been discontinued. Moreover, application of DDT created a refractory problem. Anopheles philippinensis and A. dirus are now the principal vectors resting and biting at outdoor locations. Recently incriminated malaria vectors are found resistant to DDT. Other vectors are also not amenable with this insecticide. In some areas, Malaria Control Programme (MCP) through malathion spray for vector control has produced encouraging results. In some border areas, personal protection through the use of deltamethrin-treated bed net has given quite encouraging results in controlling outbreaks of malaria. MCP until 1999 distributed about one lakh bed nets in malaria outbreak areas.
Recently the government has taken up a project with a target of treating all mosquito nets in the 13 bordering districts of the country where malaria, especially deadly cerebral malaria is most endemic with a view to bringing down malaria deaths by 50 percent within next 2-3 years.
The Directorate of Health Services is implementing this project at a cost of US dollars 24,000 funded mainly by the World Health Organisation (WHO). However the problem with the project is that only 20 to 25 percent people of the targeted areas have mosquito nets. Physicians in district and upazila hospitals, private practitioners and nurses of these areas are being given training under the project. About 150 doctors and more than 100 nurses have already been trained in the area. The hospital deaths from malaria in those areas have drastically come down to two percent from 10 percent. [SM Humayun Kabir]
Cerebral malaria' Falciparum malaria in which the brain is affected due to tendency of parasite to agglutinate, resulting in clogging of capillaries, which leads to comma or even death. Malaria has been a recognised cause of morbidity and mortality in certain parts of Bangladesh. Development of drug resistant falciparum malaria and ineffectiveness of chemoprophylaxis against falciparum have worsened the condition further. An effective reduction of vivax malaria is probably due to effective implementation of personal prophylaxis and currently administered chemoprophylaxis. Malaria has become one of the major medical problems in Bangladesh specially because of the emergence of drug resistant strains of Plasmodium falciparum. No chemoprophylactic agent appears to be effective in preventing falciparum malaria. The incidence of falciparum malaria is very high in the Chittagong Hill Tracts. In an analysis of 4,520 cases of malaria, it was found that 99% of patients suffered from falciparum malaria. Only 1% of patients were detected to have vivax variety. In this series 145 patients of falciparum malaria developed cerebral malaria; attack rate being about 4%.
A study of 102 cases of cerebral malaria conducted from January 1990 to December 1992 at Combined Military Hospital Dhaka and Chittagong, indicated maximum incidence (94%) among the people of 20 to 39 years age group. The incidence was high during May to August with a peak during June; the lowest being in November. The study revealed a significant low mortality rate of cerebral malaria with triple therapy containing quinine, cotrimoxazole and tetracycline (10.39%) when compared with quinine along with tetracycline (12.75%). Data of other prospective series of therapy also revealed that triple therapy could reduce mortality from cerebral malaria significantly compared to quinine alone. Some cases of quinine failure in falciparum malaria have been reported recently. Despite global efforts, malaria is still a highly prevalent disease in the tropics and still a major cause of death. Quinine as well as triple drug therapy have been the drugs of choice for severe falciparum malaria in Bangladesh. [Anis Waiz and Baren Chakraborty]
